When winter arrives, it’s normal for hands and feet to feel cold. However, if your fingers or toes dramatically change color—turning pale white, blue, or dark red—you might be dealing with more than just a natural reaction to chilly weather. This unusual color shift can be alarming the first time it happens, but many people eventually brush it off as a harmless quirk. In reality, these symptoms could be signs of a condition called Raynaud’s disease. While it’s not life-threatening, understanding the causes, symptoms, and when to seek medical help is essential for managing this condition effectively.

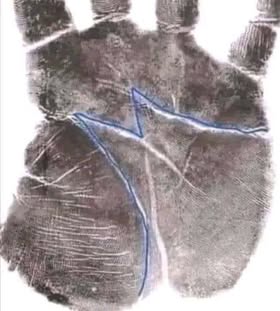
So, what exactly is Raynaud’s disease? Also referred to as Raynaud’s phenomenon, this condition affects how your blood vessels respond to cold temperatures or emotional stress. In people with Raynaud’s, the small blood vessels in the fingers and toes constrict excessively in response to cold or stress, reducing blood flow to these areas. This results in a noticeable color change, usually progressing from white to blue to red as blood flow decreases and then returns. While most people feel slightly cold in winter, individuals with Raynaud’s might experience their hands and feet becoming ice-cold and visibly discolored.
Dr. Melisa Lai Becker, speaking to Good Morning America, explains, “For most people, chilly weather might make their fingers cold, but with Raynaud’s, the hands can turn ice-cold and visibly change color.” The severity of symptoms can vary—some individuals may only experience mild discomfort, while others face significant pain and numbness that makes everyday tasks difficult.
What are the symptoms of Raynaud’s disease? The condition is most noticeable in cold weather or during periods of stress and anxiety. The primary symptoms include color changes in the fingers and toes, progressing from pale white to blue and then red as blood flow is restored. Along with these color changes, affected areas might feel numb, tingly, or painful, with sensations similar to “pins and needles.” In more severe cases, Raynaud’s symptoms can also appear in other parts of the body, such as the ears, lips, nose, and even nipples.
These symptoms typically occur in episodes, lasting from a few minutes to an hour, depending on the severity of the condition and how quickly warmth or relaxation is achieved. After an episode, the affected areas might throb, tingle, or feel swollen as blood flow returns to normal.
When should you see a doctor? While Raynaud’s is often not considered life-threatening, it can significantly impact daily life, especially if symptoms are severe or persistent. Dr. Lai Becker recommends consulting a healthcare professional if the condition starts to interfere with daily activities, such as typing, holding objects, or buttoning clothes. Persistent pain or unusually long episodes should also prompt a visit to a healthcare provider. In some cases, Raynaud’s might be linked to an underlying health condition such as lupus, rheumatoid arthritis, or scleroderma. Certain medications, including beta-blockers, migraine drugs, and chemotherapy treatments, have also been associated with Raynaud’s symptoms.
Women are more likely to develop Raynaud’s disease than men, and it often begins during the teenage years or early adulthood. Research suggests that up to 20% of adults worldwide may experience Raynaud’s to some degree. While the condition isn’t usually dangerous, complications can arise in severe cases. If blood flow is restricted for extended periods, it can lead to skin sores or, in extreme situations, tissue damage.
Managing and treating Raynaud’s disease primarily focuses on preventing attacks and minimizing discomfort. The most straightforward strategy is to keep your body warm. Wear gloves, thick socks, and layers when venturing out in cold weather. Hand warmers can also provide immediate relief during an episode. Indoors, avoid sudden temperature drops and ensure your living space remains warm.
Stress management is another critical aspect of controlling Raynaud’s episodes. Since emotional stress can act as a trigger, incorporating relaxation techniques such as deep breathing exercises, yoga, or meditation into your routine can help reduce the frequency and severity of flare-ups.
In some cases, medications may be necessary to improve blood circulation and prevent episodes. Calcium channel blockers, for example, help relax blood vessels, making it easier for blood to flow to the extremities. In more severe cases, other medications or even surgical interventions may be recommended to prevent long-term damage.
It’s important to note that if Raynaud’s is secondary to another condition, treating the underlying disease is crucial for managing symptoms effectively. Regular check-ups with a healthcare provider will help monitor your condition, track triggers, and adjust treatments as necessary.
In conclusion, Raynaud’s disease is a relatively common but often overlooked condition that can cause significant discomfort during colder months or periods of stress. While it’s not usually life-threatening, it’s essential to recognize the symptoms and take steps to manage them effectively. If you experience persistent or severe episodes, numbness, or pain, don’t ignore the signs—consulting a healthcare professional can help determine the best course of action.
By staying informed, keeping warm, managing stress, and seeking professional advice when needed, individuals with Raynaud’s can lead comfortable and active lives even during the coldest months of the year. If your fingers or toes frequently turn pale, blue, or red, don’t brush it off as just a winter quirk—it might be your body’s way of signaling an underlying issue that needs attention.